Abstract
Primary central nervous system lymphoma (PCNSL) is reported as having a dismal prognosis, due to the limited blood-brain barrier crossing capacity of lymphoma chemotherapies. Long-term remission and even cure could be achieved for a significant proportion of PCNSL patients using methotrexate-based chemotherapy regimens and intensive consolidation strategies. We report our single center experience of 27 consecutive patients with newly diagnosed PCNSL treated with Rituximab Methotrexate Temozolomide (RMT) regimen, and high-dose Etoposide Aracytine (EA) consolidation, with particular consideration for safety data.
Methods: All patients consecutively diagnosed with PCNSL from November 2013 to December 2016 at Cochin hospital (Paris, France) were retrospectively included. Primary vitro-retinal lymphoma without cerebral involvement (n=1) and immunodeficient patients (n=1) were excluded. Contrast-enhanced magnetic resonance imaging (MRI) was performed at diagnosis for all patients. Slit lamp evaluation and cerebrospinal fluid examination were performed at the diagnosis or during therapy. Induction therapy consisted of four cycles of 375mg/m² Rituximab and 8g/m² Methotrexate (with folinic acid rescue) at day 1 and 14, and Temozolomide 150mg/m² days 7 through 11, repeated every four weeks (the RMT regimen). Patients under 75 year-old without significant comorbidities and achieving a complete response (CR) or a partial response (PR) were treated with intravenous Etoposide 40mg/kg on a continuous 96h infusion days 1 through 4 and Aracytine 2g/m² twice a day days 1 through 4 (the EA regimen). MRI was performed after the second and fourth cycle of RMT and after treatment completion. Response was evaluated according to international PCNSL cooperative group (IPCG) criteria.
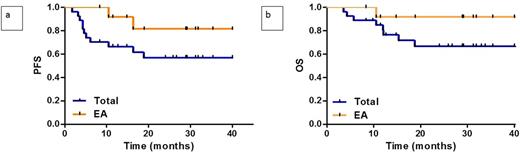
Results: Median age was 68 and 26% of the patients were under 60. Median Karnofsky performans status was 60 (range, 40-100). After induction, we observed 16 (59.3%) CR/CRu, 6 (22.2%) progressive disease (PD), 2 (7.4%) unrelated lymphoma death and 3 (11.1%) were not evaluated but were in PR after 2 cycles. Nineteen patients achieved CR/PR and were eligible for subsequent consolidation therapy. Four patients received whole brain radiotherapy (30.6 Gy n=1, 23.4 Gy n=3), and two patients had a watchful waiting strategy. Thirteen (48.1%) patients received EA. Median age of EA cohort was 60. After 29 months (range, 8-43 months) of follow-up, 19 (70.4%) patients were alive in CR. Eight patients deceased, 4 (14.8%) from progressive disease and 4 (14.8%) from lymphoma-unrelated cause. Median of progression free survival (PFS) and overall survival (OS) were not reached. The two-year PFS and OS were 57% (CI 95%, 36-74%) and 67% (CI 95%, 44-82%), respectively when considering the whole cohort; and 82% (CI 95%, 44-95%) and 92% (CI 95%, 54-99%), respectively when focusing on patients who received EA consolidation (Figures 1a and 1b). Main toxic side-effects of RMT regimen, evaluated using National Cancer Institute Common Terminology Criteria for Adverse Events V4.0 were infections (30% of grade 3-4) and liver enzymes modifications (37% of grade 3-4). We observed a single-case of fully-resolved grade 3 renal dysfunction. Regarding EA consolidation, median hospital stay and neutrophil recovery (neutrophil count over 0.5x109/l) was 22 (range, 20-183 days) and 11 days (range, 9-14 days), respectively. All patients developed grade 4 neutropenia and thrombocytopenia. Sixty one percent of patients experienced grade 3 anemia. Neutropenic fever was observed in 92.3% of patients. Grade 3-4 mucositis developed in 22.2% of patients. Sixty one percent of EA-treated patients experienced grade 3-4 infections, including documented bacterial infection in 6 patients (central venous catheter infection, n=3; septicemia, n=2 and Clostridium difficile colitis, n=1) and fungal infection in two patients (probable aspergillosis, n=1 and documented mucormycosis, n=1). We observed one case of vancomycine-induced grade 4 renal failure during febrile aplasia that fully recovered.
Conclusion : The RMT regimen allowed a near 60% complete response rate with limited toxicity. Intensive Etoposide Aracytine consolidation is feasible but more toxic than previously reported. The high survival rate observed in patients receiving RMT induction and then EA consolidation support further comparative evaluation of this strategy in prospective trials.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal